The percentage of teenagers who were up to date on their human papillomavirus (HPV) vaccines has fallen dramatically since 2020, according to new federal data released Thursday.
The Centers for Disease Control and Prevention (CDC) currently recommends children from ages 11 to 12 receive two doses of the HPV vaccine, given six to 12 months apart, although children can get the vaccine starting at age 9.
Anybody under age 26 can get the HPV vaccine if they have not been fully vaccinated, according to the CDC. People ages 15 to 26 years old who have not received the HPV vaccine typically need three doses to be fully vaccinated.
The CDC’s report looked at data from the 2023 National Immunization Survey -Teen, a group of phone surveys used to monitor vaccination coverage among teenagers. Similar ones are conducted for children and adults.
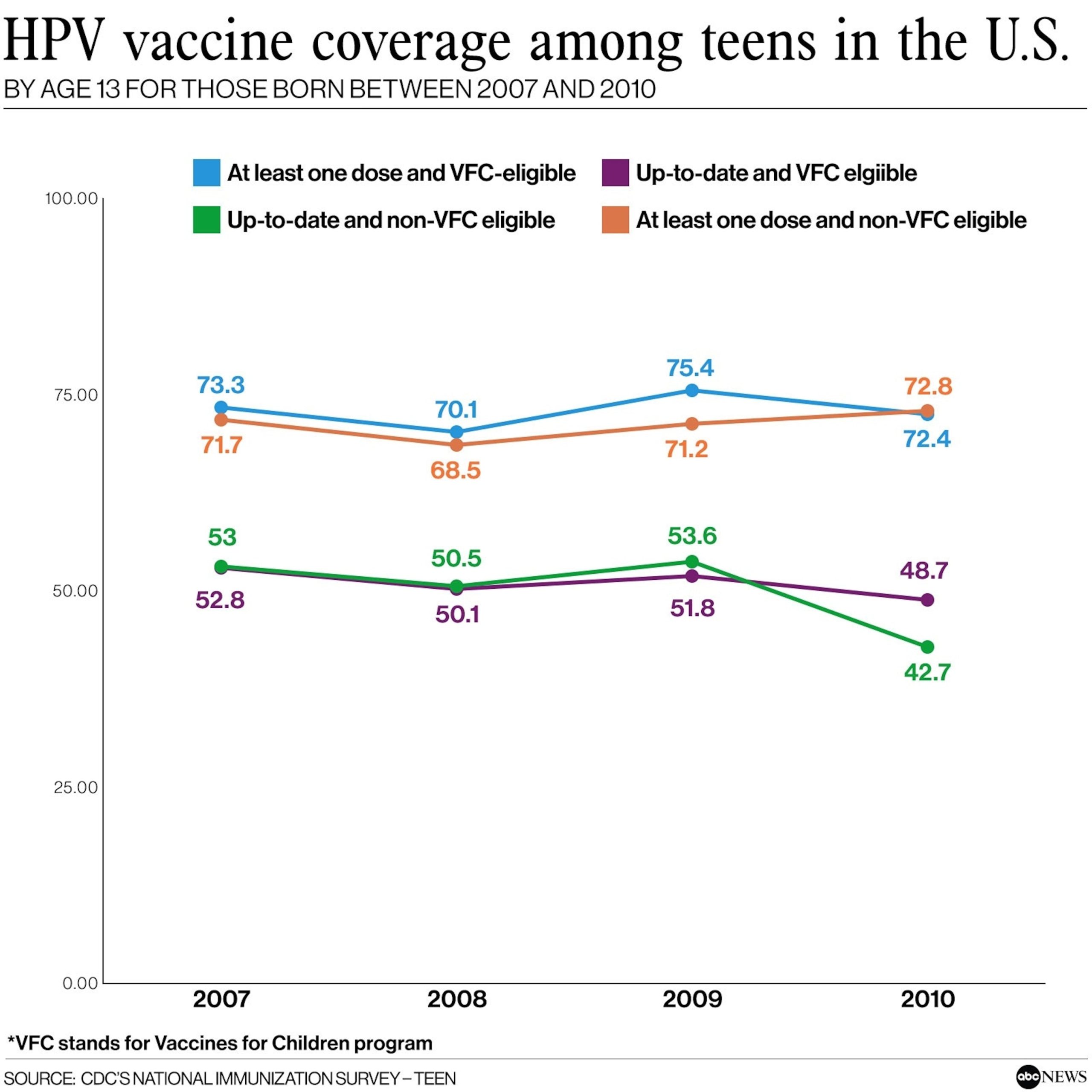
The survey looked at trends in coverage by birth year, and trends in coverage by eligibility for the Vaccines for Children (VFC) program, a federally funded program that provides vaccines to children whose parents or guardians may not be able to afford them.
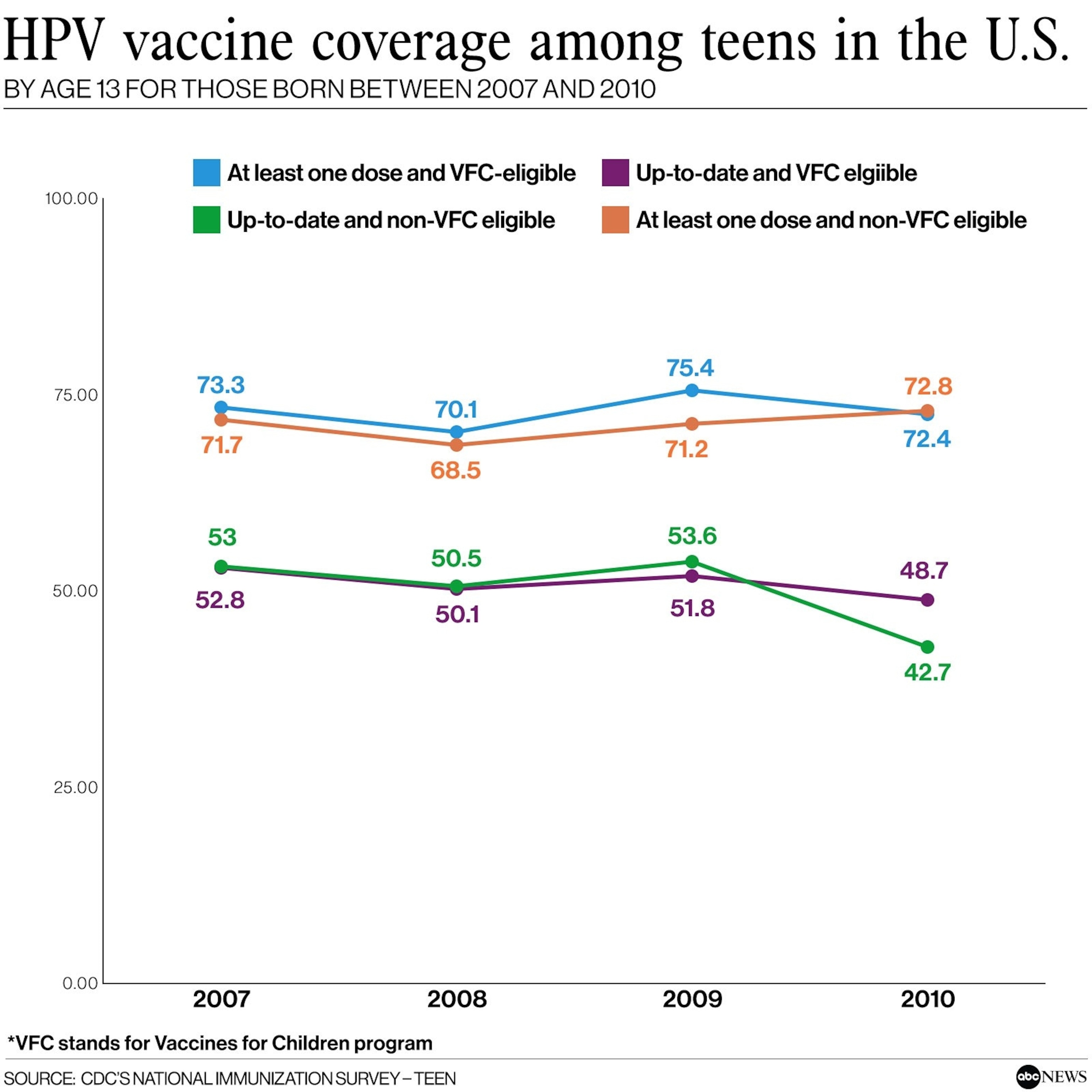
HPV vaccine coverage among teens in the U.S. By age 13 for those born between 2007 and 2010
CDC’s National Immunization Survey – Teen
The program found that vaccination coverage for vaccines including tetanus, diphtheria, and acellular pertussis vaccine (Tdap), as well as for the meningococcal ACWY vaccine, was generally stable during the COVID-19 pandemic.
However, there was a notable decrease in the percentage of adolescents who were up to date with HPV vaccination by age 13 among those born in 2010 — who would have turned 13 in 2023 — compared with those born in 2007, who would have turned 13 in 2020.
For teens who were born in 2007, 52.8% of those who were not eligible for VFC were up to date on their HPV vaccines by age 13. By comparison, only 48.7% of non-eligible teens born in 2010 were up to date by age 13.
Among teens born in 2007 who were VFC eligible, 53% were up to date by age 13. However, only 42.7% of eligible teens born in 2010 were up to date by age 13.
“The decline in the percentage of VFC- eligible adolescents who are HPV [up to date] could signal a change in accessibility to vaccination through the VFC program, a change that needs further exploration,” the report read. “This possibility under-scores the importance of ongoing efforts to ensure equitable access to vaccination services for all children and adolescents.”
Overall, 2023 coverage was similar to 2022, with 76.8% of all teens between ages 13 and 17 receiving at least one dose of the HPV vaccine compared to 76.0% in 2022, the report found.
However, only 61.4% of all teenagers in this age group were updated on their HPV vaccines, down from 64.6% in 2022.
HPV is a very common STI that infects about 13 million Americans each year, according to the CDC. Nearly everyone will contract HPV at some point in their lives, the CDC says.
There are more than 100 types of HPV, and most HPV infections clear up on their own within two years.
About 10% of infections last longer and can put individuals at risk for some cancers including cervix, vaginal and vulvar cancer; penile cancer; anal cancer; and oropharyngeal cancer, which is a cancer of the back of the throat, according to the CDC.
Every year, HPV causes about 37,000 cases of cancer in both men and women in the U.S., according to the federal health agency. However, HPV vaccination can prevent more than 90% of HPV cancers when given at the recommended ages, according to the American Cancer Society.
“Health care providers should make strong recommendations for all routine vaccines and verify if adolescents, particularly those eligible for the VFC program, are up to date with all recommended vaccines,” the report stated.
The Centers for Disease Control and Prevention (CDC) recently released a report that has raised concerns about the declining rates of HPV vaccine coverage among teenagers since 2020. The report, which analyzed data from the National Immunization Survey-Teen, found that there has been a significant decrease in the number of adolescents receiving the recommended doses of the HPV vaccine.
HPV, or human papillomavirus, is a common sexually transmitted infection that can lead to various types of cancer, including cervical, anal, and oropharyngeal cancer. The HPV vaccine is highly effective in preventing these cancers, yet vaccination rates have been steadily declining in recent years.
According to the CDC report, in 2020, only 51% of adolescents aged 13-17 had received all recommended doses of the HPV vaccine, down from 54% in 2019. This decline is particularly concerning given the potential impact on public health. Without adequate vaccination coverage, more individuals are at risk of developing HPV-related cancers later in life.
There are several factors that may be contributing to the decline in HPV vaccine coverage among teens. One possible reason is misinformation and misconceptions about the vaccine. Some parents may be hesitant to vaccinate their children due to concerns about safety or efficacy. However, numerous studies have shown that the HPV vaccine is safe and effective at preventing HPV-related cancers.
Another factor that may be influencing vaccination rates is the ongoing COVID-19 pandemic. The pandemic has disrupted routine healthcare services, including vaccination programs. Many adolescents may have missed out on their scheduled HPV vaccines due to lockdowns, school closures, and other pandemic-related challenges.
To address the decline in HPV vaccine coverage among teens, it is crucial for healthcare providers, public health officials, and community leaders to prioritize vaccination efforts. This includes raising awareness about the importance of the HPV vaccine, dispelling myths and misinformation, and ensuring that adolescents have access to vaccines through school-based programs, healthcare providers, and community clinics.
It is also important for parents to have open and honest conversations with their children about the benefits of the HPV vaccine and the importance of protecting themselves against HPV-related cancers. By working together to increase vaccination rates, we can help prevent unnecessary suffering and save lives from preventable cancers.